Unless you are at risk for any complications, you will likely be going home the same day you have surgery. Before going home, the doctors and staff will ensure you can get up and walk with an assistive device, which will most likely be a walker. Depending on your doctors’ preferences, you will likely either start in the physical therapy clinic the day after surgery or have several weeks of therapy at home before outpatient physical therapy in a clinic.
For patients without nursing needs, getting your therapy started in the convenience of your home may be preferable. Therapists will address your ability to safely access your home and navigate stairs, start you on an exercise program and provide techniques for managing your post operative pain and swelling. Athletico now offers home therapy in many areas of the country. Refer to the home therapy page on the Athletico website to request home therapy.
It is important to be aware that you may experience some pain after surgery. Your physician may prescribe you pain medication as needed and guide you on when to take it to maximize your rehabilitation potential during therapy sessions. In addition, swelling and bruising in the knee area are normal! You may even have some swelling near the hip or in the foot/ankle, as a tourniquet is used to decrease bleeding during surgery and due to gravity., in addition to swelling at the
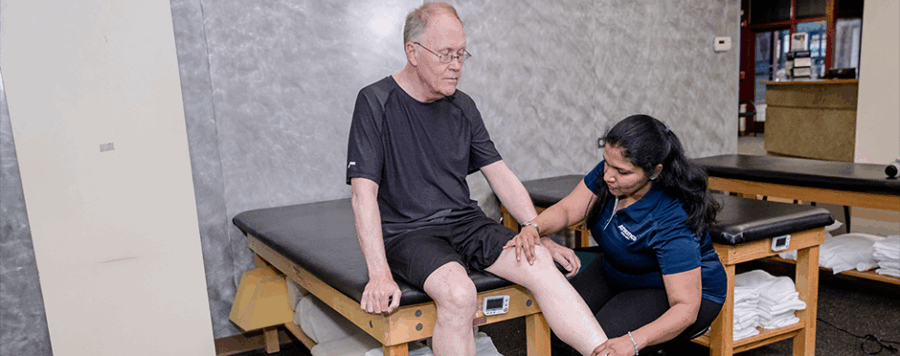
After your home care ends, you will likely transition to care at the clinic. Your evaluation will consist of your therapist getting to know your situation, obtaining measurements of range of motion and strength, observing walking and transfer mechanics, and developing a home exercise program and plan of care to get you back to where you want to be.
What kinds of things will you do during follow-up physical therapy visits? Your therapy sessions will focus on activities that assist with knee bending, straightening, strengthening, and manual therapy. Scar tissue formation can reduce your knees’ ability to bend and straighten, so focusing on getting your motion back is important! I like using the stationary bike or nu-step to warm up and get the knee bending. In addition, your therapist may utilize therapy techniques to promote mobility of both bending and straightening, reduce scar tissue restrictions, and reduce swelling. In addition, Exercises will be included in your plan of care to focus on promoting the strengthening of the knee, like small-range squats or steps. Cues may also be given to help improve walking. Following each session, your therapist may suggest a modality such as ice or electrical stimulation to help reduce swelling and pain.
There are a few milestone moments that we look for in therapy:
- Achieving full knee extension. This allows you to walk with normal mechanics (no limping!)
- Walking without limping without an assistive device
- Achieving 90 degrees of knee flexion. Your goal should be to achieve at least 90 degrees of knee bending within the first several weeks of therapy.
- Achieving 120 degrees of knee flexion. Studies say this is the goal motion after knee replacement. We like it when you’re able to get even more!
- Strong enough to go up and down stairs reciprocally with control
The duration of outpatient physical therapy following a knee replacement can range between 2-5 months, depending on how quickly your recovery occurs. This means that your range of motion and strength are to a point where you can continue your exercises on your own and are safe with daily activities. It is important to know that it can take between 6 months to a year to feel “normal.” This does not mean you won’t be able to do everything you want before this. There will be days where you get some soreness more than others, but this will be far less often and less intense as it is closer to the start of care.
To ensure you are in a better position to recover from your knee replacement, consider doing physical therapy before surgery. Improvements in strength and range of motion before surgery can help put you in an even better position post-surgery. Working on strength and range of motion can also reduce your overall pain symptoms and may put off the need for surgery for some time.
Physical Therapy Can Help
If you have more questions about managing your recovery post-surgery, setting up pre-operative physical therapy, or to learning more about Home Therapy options, please contact your local Athletico clinic and schedule a free assessment. Free assessments are available in-clinic and virtually through our telehealth platform.
*Per federal guidelines, beneficiaries of plans such as Medicare, Medicaid, Tricare, VHA and other federally funded plans are not eligible for free assessments.
The Athletico blog is an educational resource written by Athletico employees. Athletico bloggers are licensed professionals who abide by the code of ethics outlined by their respective professional associations. The content published in blog posts represents the opinion of the individual author based on their expertise and experience. The content provided in this blog is for informational purposes only, does not constitute medical advice and should not be relied on for making personal health decisions.
Peter Batz is a Doctor of Physical Therapy specializing in orthopedics, vestibular therapy, headache/TMD, dry needling, ACL rehabilitation, and injury prevention. Peter graduated from Northern Illinois University with a Doctorate in Physical Therapy. He also completed an orthopedic residency through Evidence in Motion and obtained his Orthopedic Certified Specialist (OCS). He strives to get his patients back to performing at their peak levels so they can enjoy life to the fullest.

 width="900"
height="356"
>
width="900"
height="356"
>
