TMD: Differences in Women vs. Men
Leave a CommentThe comparison between women and men is a common one, and the medical world is no exception. Many dysfunctions and diseases are statistically greater in one gender over the other, including Temporomandibular Dysfunction (TMD).
TMD affects around 12 percent of the world population and 35 million people in the United States. Although TMD affects both men and women, the majority of those seeking care are women ages 19-49. In fact, TMD is diagnosed in women five times more frequently than men. Women also tend to have more severe symptoms, with data showing women are nine times as likely to be diagnosed with major limitations in jaw movements and chronic, unremitting pain.1,2
Why are women impacted by TMD more often than men?
There are many theories as to why TMD occurs more often in women versus men. Hormonal, anatomic, behavioral, and genetic differences have been linked to the disproportional ratio of women to men diagnosed.2,3,4
Hormonal differences between the genders have been implicated as TMD is diagnosed more often in women during childbearing years when estrogen and progesterone levels are higher. During the menstrual cycle, there is evidence that ligament laxity increases during the pre-ovulatory phase when estrogen dominates. The hormone relaxin is secreted during the follicular phase (days 1-9) and peaks during the luteal phase (days 15-28). Typically laxity is the highest during the luteal phase. Although the specific hormones released are the same with each phase, the level of these hormones varies among women causing some women to experience greater laxity related symptoms than others. As ligament laxity increases, joint play increases and joints can become irritated.2
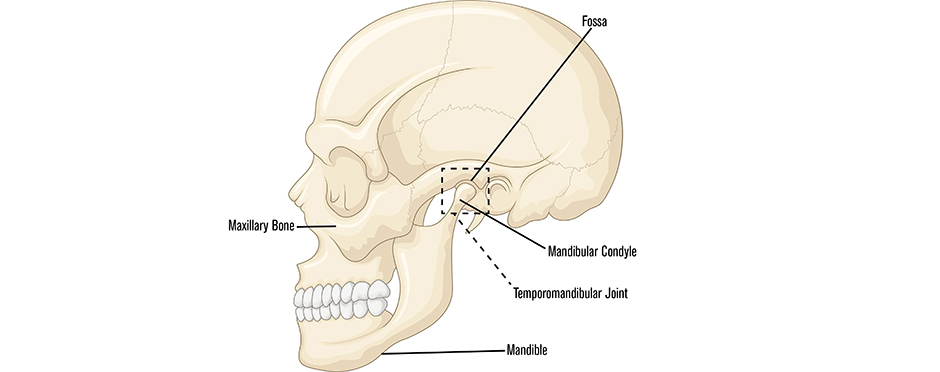
Additionally, anatomical differences across males and females in both the jaw and skull affect the forces on the temporomandibular joint (TMJ). For example, the maxillary or upper jaw bones in males are longer, wider and thicker than in females. The angle created by the top and bottom of the mandible or lower jaw is less obtuse than the female mandible. The mandibular condyle or head is larger and the temporal fossa/socket is deeper. All of these anatomical factors create a more stable environment for TMJ translation.4
Behaviorally, differences in stress management between women and men can be linked to the occurrence of several factors involved with TMD. Clenching, bruxism (grinding), and poor breathing habits can all increase with the internalization of stress. Consequently, these habits can then increase stress and irritation of the TMJ.3
Lastly, a particular gene variant has been shown to increase sensitivity to pain. This variant has been found to be more prevalent among people with TMD than without. Scientists have also found that most patients with TMD experience pain in other areas. The simultaneous presence of two chronic conditions in a patient, known as comorbidity, is more commonly diagnosed in women. Comorbid diagnoses may include chronic fatigue syndrome, chronic headache, endometriosis, fibromyalgia, interstitial cystitis, irritable bowel syndrome, low back pain, sleep disorders and vulvodynia. These diagnoses are considered comorbidities because they occur in combination with TMD more often than chance can explain.2,3,4
Because pain is a common link in the aforementioned conditions, National Institute of Health (NIH) scientists are seeking to understand the pain process and are exploring differences between men and women in how they respond differently to pain and pain medications. Scientists hope to explain the common mechanisms between facial pain in TMJ disorders and other pain conditions.2,3
Living with TMD
Research indicates that TMD is a complex disease involving hormonal, anatomic, behavioral and genetic components. As with many disease processes, the differences between men and women affect the outcomes. With TMD specifically, women are more greatly affected by their differences in these areas.
If you are living with TMD, it is important to note that physical therapy can be a treatment option. Hands-on treatments and exercise can lead to improved movement of the TMJ, reducing pain and increasing mobility. If you are experiencing facial or jaw pain, click the button below to schedule an appointment at an Athletico location near you.
The Athletico blog is an educational resource written by Athletico employees. Athletico bloggers are licensed professionals who abide by the code of ethics outlined by their respective professional associations. The content published in blog posts represents the opinion of the individual author based on their expertise and experience. The content provided in this blog is for informational purposes only, does not constitute medical advice and should not be relied on for making personal health decisions.
1. “TMJ Association, Ltd.” TMD BASICS | TMJ.org. N.p., n.d. Web. 23 Jan. 2017. <http://tmj.org/site/content/tmd-basics>.
2. “TMJ Disorders.” National Institute of Dental and Craniofacial Research. N.p., n.d. Web. 23 Jan. 2017.
3. Pain. Analysis of gender effects on pain perception and symptom presentation in temporomandibular pain. 1993 Apr;53 (1):73-80.
4. “Identification of Pathological Conditions in Human Skeletal Remains.” 5 Nov. 2010, doi:10.1016/b978-0-12-528628-2.x5037-6.
